SYLLABUS
GS-2: Issues relating to development and management of Social Sector/Services relating to Health.
Context: Recently, WHO has issued its first-ever clinical guidelines recommending GLP-1 therapies for the treatment of obesity in adults, marking a major expansion beyond earlier recommendations limited to Type II diabetes.
Key WHO Guidelines on GLP-1 Therapies for Obesity
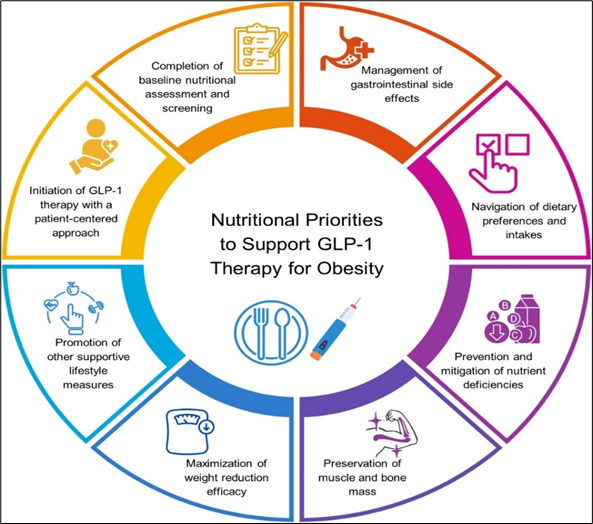
- GLP-1 medications must be paired with evidence-based behavioural interventions, including healthy diets and physical activity.
- In adults living with obesity, GLP-1 therapies may be used as a long-term treatment for obesity.
- In adults living with obesity who are prescribed GLP-1 therapies, intensive behavioral therapy may be provided as part of a comprehensive multimodal clinical algorithm.
- The recommendation is “conditional”, reflecting limited long-term data on efficacy, safety, maintenance, discontinuation, and high current costs.
- The therapies should not be used in pregnant women.
Challenge of Ensuring the Medication and WHO recommendations:
- Major global accessibility inequity: The United States currently consumes nearly 75% of global GLP-1 supply.
- Limited Reach: Even with expanded production, GLP-1 drugs may reach only 10% of eligible adults worldwide in the next five years.
- WHO recommends expanding access through strategies such as:
- Pooled procurement
- Tiered pricing
- Voluntary licensing to local manufacturers
Global Policy Implications
- The new guidelines go beyond the WHO Essential Medicines List (EML), where GLP-1 drugs were previously listed only for diabetes treatment.
- Countries where obesity drugs are not yet approved will need to re-evaluate regulatory frameworks and treatment policies.
- Rising obesity rates in low- and middle-income countries raise concerns about access gaps, especially where even basic diabetes care remains limited.
- Demand is expected to grow significantly in the European Union, China, and India.
About GLP-1 therapies
- GLP-1 therapies (glucagon-like peptide-1 receptor agonists) are a class of medications that mimic the natural GLP-1 hormone, which helps regulate blood sugar and appetite.
- GLP-1 medicines stimulate insulin release when blood sugar is high and reduce glucagon secretion, helping lower blood glucose levels.
- They slow down the process of food digestion and increase feelings of fullness, leading to a reduction in food intake.
- It functions both as an incretin hormone and a neurotransmitter, and is secreted from the small intestine and the hindbrain after a meal.
- It travels to the pancreas, where it regulates blood sugar by increasing insulin and decreasing glucagon. This is referred to as the incretin effect.
- This effect is blood glucose-dependent, meaning it occurs only when blood glucose levels are elevated.
- It also influences centres in the brain associated with hunger and satiety, effectively signalling that we have eaten enough and should stop.
- GLP-1 binds to receptors located in many organs throughout the body.
- It also produces beneficial effects in organs such as the kidney, liver, and cardiovascular system.

